Coxiella burnetii, the bacterium responsible for Q fever, is a unique and highly infectious pathogen that presents considerable challenges to public health systems worldwide, including in North America. Unlike many other bacteria that cause foodborne illnesses, C. burnetii is most commonly transmitted to humans through inhalation of dust contaminated by infected animal excretions or via contact with the milk, meat, or wool of infected animals. This blog post aims to explore the complex nature of C. burnetii, its transmission dynamics, the health burden it imposes, and the strategies for prevention and control.
Biology and Epidemiology
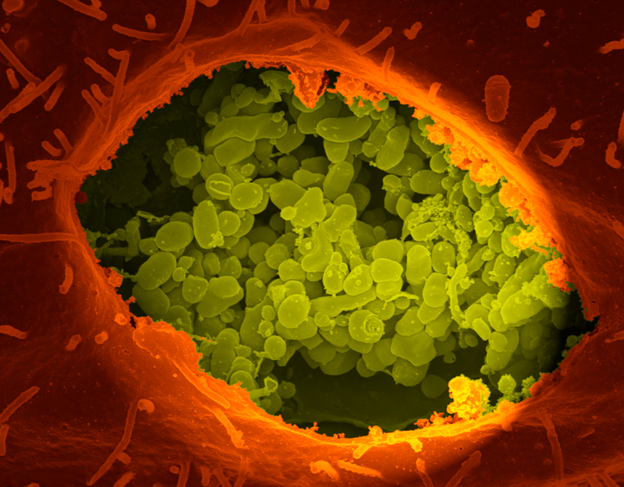
C. burnetii is an intracellular pathogen capable of surviving in extreme conditions for extended periods, partly due to its spore-like phase, which is highly resistant to heat and desiccation. This resilience facilitates its spread and complicates efforts to control the bacterium. Q fever can manifest in acute or chronic forms, with symptoms ranging from mild flu-like illness to more severe manifestations, including pneumonia and hepatitis. Chronic Q fever, although less common, can lead to endocarditis, posing significant health risks.
Prevalence and Public Health Impact
In North America, Q fever cases have been reported across various regions, with incidence rates fluctuating over the years. The actual number of cases is likely underreported due to the nonspecific symptoms associated with the disease, leading to misdiagnosis or underdiagnosis. Agricultural workers, veterinarians, and individuals in close contact with animals are at a higher risk of exposure. The economic impact of Q fever is significant, encompassing healthcare costs, loss of productivity, and implications for animal husbandry practices.
Challenges in Detection and Control
One of the primary challenges in managing Q fever is its diverse transmission routes, including airborne spread, which can lead to outbreaks among humans without direct contact with animals. The detection of C. burnetii requires specialized laboratory tests, often involving PCR or serology, which may not be readily available in all healthcare settings. Control measures are further complicated by the bacterium's resilience in the environment and the wide range of animal reservoirs.
Prevention Strategies
Effective prevention and control of Q fever involve a multifaceted approach:
- Surveillance and Reporting: Enhanced surveillance systems and prompt reporting of cases can help identify outbreaks early and inform public health responses.
- Vaccination: Vaccines for Q fever are available in some countries and can be offered to high-risk populations, including animal workers and veterinarians.
- Public Health Education: Raising awareness about Q fever among at-risk groups and the general public is crucial. This includes education on the importance of personal protective equipment (PPE) and safe animal handling practices.
- Environmental Management: Strategies to reduce the risk of C. burnetii transmission include proper disposal of birth products in farms, dust control measures, and pasteurization of dairy products.
The Way Forward
Advancements in diagnostic techniques, vaccine development, and public health strategies are critical for reducing the burden of Q fever. Ongoing research into the ecology of C. burnetii and the factors influencing its transmission will be essential for devising effective prevention and control measures. Collaboration between human and veterinary health sectors, known as a One Health approach, is pivotal in managing Q fever and mitigating its impact on public health.
Conclusion
Coxiella burnetii poses a unique challenge to public health due to its resilience, diverse transmission routes, and the potential for severe disease outcomes. By implementing comprehensive strategies that encompass surveillance, vaccination, public education, and environmental management, we can protect vulnerable populations and minimize the public health impact of Q fever in North America and beyond.
